Acne scarring presents a challenging aesthetic problem to the aesthetic practitioner. According to the available evidence, what types of laser have been shown to be more appropriate and why? Discuss your options in relation to patient, scar, technology and side effects.

Dr MJ Rowland-Warmann BSc BDS MSc Aes.Med. PGDip Endod. MJDF RCS (Eng)
For her MSc Masters Degree in Aesthetic Medicine for the Queen Mary University of London. The following essay received a Distinction – the highest mark awarded.
This is an academic essay. If you are a patient seeking treatment from one of Liverpool’s most learned aestheticians then take a look at our main treatments pages here:
Lip Fillers | Plexr Soft Surgery | Botox Treatment

Acne is very common, occurring in 80% of 11-30 year-olds and leaving permanent, disfiguring scars (8), which can affect personal perception and be a source of social stigma (16). Many treatments for acne scarring have been developed with varying success rates. Laser treatments offer promising, permanent solutions for those affected.
Acne Scars
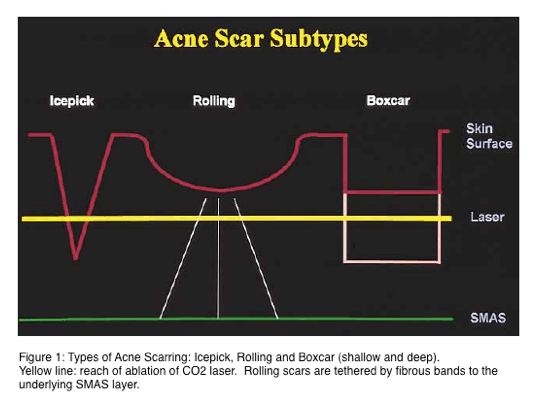
Scars are either hypertrophic or atrophic (2). Hypertrophic scars occur due to increased collagen synthesis at the original wound site with lack of collagen lysis, remaining within the confinement of the original damaged area (16). Atrophic scarring seen in acne can further be divided into ice-pick, rolling and boxcar (2,8).
Ice-pick scars are less than 2mm, narrow and deep, with sharp margins. Rolling scars occur due to the destruction of subcuticular fat and subsequent anchoring of the dermis to the subcutis, displaying tethering. Both of these types are often difficult to treat with most lasers. The third type of commonly seen acne scar is boxcar, a sharply demarcated scar which can be shallow or deep, the same width at the base and surface, and which can respond well to laser treatment (8,12). Acne scars display epidermal thinning and have disorganised collagen fibre networks (9), which can manifest in skin texture changes (13).
Figure 1 illustrates the different types of acne scarring (reproduced from 8). Boxcar scars can be subdivided into shallow and deep. For reference, the yellow line indicates the depth of ablation for a CO2 laser, to be discussed forthwith.
Types of Lasers for Acne Treatment
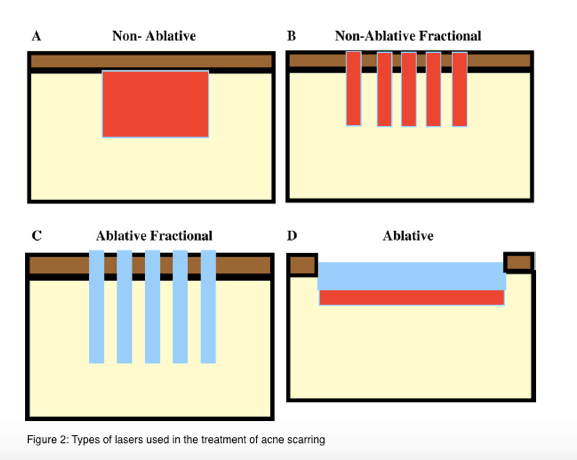
Light amplification by stimulated emission of radiation systems, or LASERS, target specific tissue chromophores such as water, haemoglobin and melanin resulting in selective photothermolysis, a theory that was proposed by Anderson and Parrish in 1983 (7,13). The target chromophore absorbs the laser wavelength more than the surrounding tissues, causing targeted destruction to treat an array of skin irregularities (3,7). There are four basic types of tissue interaction seen with lasers: non-ablative, non-ablative fractional, ablative fractional and ablative (1). Wavelength selection to suit the target chromophore and choice of thermal damage pattern are essential to bring about the desired response and improve the appearance of acne scars.
Figure 2 illustrates the types of lasers available (1).
Non-ablative lasers (NA)
Non-ablative lasers cause heating of the skin beneath the epidermis, causing thermal injury but sparing the epidermal cover, with minimal downtime (1,11). NA treatment stimulate neocollagenesis, seen at around 6 months, by inducing production of type I and III collagen and elastic fibres in the dermis to bring about improvement (4,5,9).
585-Pulsed Dye Laser (PDL)
Popular for use in light acne scarring, this NA treatment can be used for patients with Fitzpatrick (FP) skin types 1 and 2 only due to the competition with melanin and potential for Postinflammatory Hyperpigmentation (PIH).
1064 Nd:YAG
A NA remodelling laser, it has significantly more effect than PDL and is effective in stimulating collagen. Due to the decreased absorption of melanin, this laser is safer for use in higher FP types (13). Combining PDL and Nd:YAG has been shown to bring about an improvement in scar appearance of 40-50%. Due to the fact that ice-pick scars respond better to PDL and boxcar scars respond more favourably to Nd:YAG, their combination can significantly improve scarring (9).
1320nm Nd:YAG, 1450nm diode and 1540nm Er:Glass
These mid-infrared lasers have no effect on skin colour, redness or pigmentation as they are not absorbed by melanin or haemoglobin and therefore can be used in high FP groups. Er:Glass lasers have shown improvement in scars of 20-30% (5). The main advantage to NA lasers is the minimal side effect profile and reduced discomfort. These lasers are popular, but their capability to treat acne scarring is limited to fine and moderate scars with a requirement for multiple treatments (5,10).
Non-ablative fractional lasers (NAF)
Fractional lasers create columns of thermal damage, known as micro-thermal treatment zones (MTZ), whilst leaving the epidermis intact (1,6). MTZ can reach a depth of 300-400 microns in the dermis and induce collagen remodelling (6). They include lasers such as 1550nm Er:Glass. Side effects of NAF include post-operative discomfort, oedema and flaking. Risks of NAF are less than with ablative resurfacing, but can still result in crusting, scarring and, especially in higher FP types, PIH (1). Generally, several sessions of treatment will be required in order to achieve results (1). Few studies have shown effects of NAF for use in acne scarring, but a study conducted by Shin et al showed that there was no difference in outcome between NAF and AFL in the treatment of surgical scars (6).
Ablative fractional laser (AFL)
First developed in 2004, fractional resurfacing has revolutionised acne scar treatment (10). AFL creates thermal ablation of MTZ of epidermal and dermal tissue in regularly spaced columns whereby 15-20% of the surface is treated resulting in deep dermal damage of up to 700 microns (11). The adjacent skin to these MTZ is left untreated, acting as a healthy cells reservoir and resulting in fast healing, collagenesis and a short recovery with re-epithelialisation is as little as 48 hours (5,10). Due to this, side effects are lower than for ablative lasers and results can be comparable (4).
10600nm CO2 (Carbon Dioxide)
This AFL creates both coagulation and ablation (5), its MTZ depth can be as deep as 300 microns to 1mm (4). There is a high risk of PIH with fractionated CO2 lasers. In FP types 3 and 4, PIH has been reported as high as 55.5% in one study (4). In a study by Hsiao, 24% of the subjects exhibited PIH at one month (15), whereas when considering studies with asian subjects, whilst demonstrating a 25-50% improvement in 85% of subjects, PIH was found to be present in 92% of the patients. Whilst this figure is high, adjunct treatment with bleaching creams such as 4% Hydroquinone reduced this significantly after 5 weeks (14). Whilst the rates of PIH in fractionated CO2 treatment are lower than for fully ablative treatment, there is a need for repeated treatments to achieve the same level of scar improvement.
2940nm Er:YAG (Yttrium-aluminum-garnet)
This AFL demonstrates pure ablation on treatment and results show 25-50% improvement in scars (10). Due to the closeness of wavelength to the water absorption coefficient at 3000nm, almost all energy is absorbed into the dermis, causing less thermal damage. Treatment with Er:YAG is less successful than with AFL CO2, but with a decreased side effect profile and shortened recovery time (5). There is a trade-off between effectiveness of scar reduction and downtime, in that repeated treatments will be required to achieve the same effect. Due to the depth of penetration possible with fractionated lasers, they can help to detach tethering under atrophic scars and bring about improvement (12)
Ablative Lasers
Ablative lasers, such as CO2 and Erbium:YAG, are the gold standard in treatment of acne scars (7), removing the epidermis and cause thermal damage to the dermis by using water as the chromophore (1,5), causing rapid heating and vaporisation of tissue (3). They cause significant side effects and downtime due to the removal of the epidermis and can result in pain, oedema, oozing, infection, scarring and pigment changes (1).
10600nm CO2
This far infrared spectrum laser causes penetration of 20-30 microns in the zone of ablation and a broad zone of residual thermal damage (RTD) of up to 200 microns (4,5,7). The RTD results in heat-mediated contraction and subsequent collagen remodelling, which leads to the dramatic skin tightening effect seen after treatment (3). Riggs et al demonstrated 69% improvement in the appearance in acne scarring at 1 month, with further increased improvements within an 18-month follow-up period due to dermal remodelling (3). Ice-pick, boxcar and hypertrophic scars respond well to treatment with ablative CO2 and improvement of up to 81.4% has been demonstrated in moderate to severe acne scarring (10).
There is a high rate of PIH in ablative CO2 laser treatment, reaching 21-45% in caucasian patients of FP type 1 and 2 (4,7) and increasing to 50% in FP type 3. A study by Triana et al on patients with latino skin showed 30.4% PIH was observed, but with satisfaction rates of 86.7%, suggesting good results with acceptable rates of complication (7). Hypopigmentation can also occur, and has been documented at 8-19% (3).
Due to the fully ablative nature of treatment with involvement of both epidermis and dermis, there are short and long term side effects to treatment with this type of laser. Skin fragility, peeling and redness can last up to three months, with milia and acneiform eruptions documented in up to 84% of patients. Infections can occur due to inadequate post-operative wound care, and hypertrophic scarring can occur as a delayed response, observed in around 2-3% (3).
2940nm Er:YAG
Another far infrared spectrum laser, Er:YAG has an absorption coefficient close to water, resulting in penetration depths of 1-3 microns per J/cm2 and RTD of 10-40 microns (5) and therefore less underlying thermal damage, meaning shorter healing times (3). Due to the decreased RTD, however, there is less collagen shrinkage after treatment, resulting in less pronounced effects. This also means that several passes can be made in treatment without severe side effects and significant RTD increase (3).
Similar to ablative CO2 treatment, Er:YAG is useful for the treatment of ice-pick scars, shallow boxcar scars and some hypertrophic scars (13). The mean improvement is around 40% (10). Compared with ablative CO2 treatment, the healing time of single pass Er:YAG treatment is reduced. However, when comparing single pass CO2 with multiple pass Er:YAG, similar recovery periods and re-epithelialisation rates have been documented with no long term side effects. The number of passes and treatment sessions required will be dependent on the severity of scarring.
Not free of side effects, hyperpigmentation rates of up to 38% were reported with high pulse rates. Shortened pulse rates have resulted in a reduced risk of pigmentary disturbance and Er:YAG ablative treatment can be considered safer in the treatment of higher FP types than CO2 ablation. Other side effects included acneiform eruptions, milia and dermatitis (3,11). Both CO2 and Er:YAG treatment recovery can take several months depending on treatment intensity.
Ablative versus AFL CO2
It is not disputed that ablative CO2 laser incurs higher rates of complication than AFL. Erythema in ablative resurfacing is 64% compared with 9.7% in AFL, oedema is higher at 25.4% compared with 4.8% in AFL, and pain scores were demonstrated at 20% in ablative resurfacing, whereas AFL showed 10% (7). PIH is always a worry when treating patients with lasers. Whilst the results obtained with ablative CO2 lasers are outstanding, risks of PIH are significantly higher compared with AFL. Triana et al illustrated the rates of PIH in various FP groups in Table 1.
Table 1: Comparison of PIH in ablative versus AFL CO2 laser treatment.
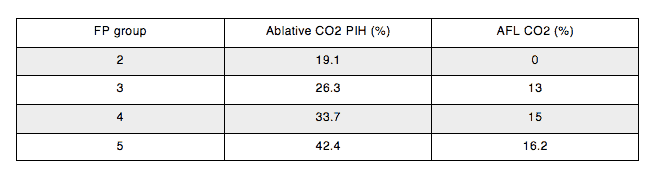
Other studies have shown similar outcomes, with 37% incidence PIH in all FP types, increasing to 70% in FP 4 or higher (14). Whilst it would be beneficial to the patient to avoid any incidence of PIH, given that the stigma of acne scarring is an aesthetic hindrance, successful treatment of PIH can be achieved with topical Hydroquinone and retinol, which has shown to bring about 90% resolution in 4 months (7).
Conclusion
In the treatment of acne scars, it is important to choose a laser treatment modality that can treat all types of acne scar in order to bring about an improvement in the aesthetic concerns of the patient. Choosing the correct laser treatment needs to take into consideration scarring severity, skin type and downtime, especially with regard to patient motivation. Patients whose psychological status has already been affected by scarring may not be ideal candidates for a lengthy recovery period. The gold standard treatment with ablative CO2 lasers, whilst delivering excellent scar improvement and skin texture results, may not be appropriate for all patients, especially high FP types at risk of PIH, so a compromise that allows a good resolution with manageable side effects is often preferable. It is important to acknowledge that no treatment can completely remove scarring, but that laser treatments can significantly reduce morbidity associated with skin irregularities after acne.
References
- Tannous Z; Fractional resurfacing. Clinics in Dermatology (2007)25, 480-486
- Jemec GBE, Jemec B; Acne: Treatment of Scars. Clinics in Dermatology (2004)22, 434-438
- Riggs K, Keller M, Humphreys TR. Ablative laser resurfacing: high-energy pulsed carbon dioxide and erbium:yttrium-aluminum garnet. Clinics in Dermatology (2007)25, 462-473
- Chan N, Ho S, Yeung C, Shek S, Chan H; Fractional Ablative Carbon Dioxide Laser Resurfacing for Skin Rejuvenation and Acne Scars in Asians. Lasers in Surgery and Medicine (2010)42, 775-783
- Lipozencic J, Bukvic Mokos Z; Will nonablative rejuvenation replace ablative laser and controversies. Clinics in Dermatology (2013)31, 718-724
- Shin JU, Gantseteg D, Jung JY, Jung I, Shin S, Lee J; Comparison of Non-Ablative and Ablative Fractional Laser Treatments in a Postoperative Scar Study. Lasers in Surgery and Medicine (2014)46, 741-749
- Triana L, Cuadros S, Triana C, Barbato C, Zambrano M; Laser Resurfacing for Latin Skins: The Experience with 665 Cases. Aesthetic Plastic Surgery (2015) Epub ahead of print
- Jacob CI, Dover JS, Kamin MS; Acne scarring: a classification system and review of treatment options. Journal of American Academy of Dermatology (2001)45, 109-117
- Lee DH, Choi YS, Min SU, Yoon MY, Suh DH; Comparison of a 585-nm pulsed dye laser and a 1064-nm Nd:YAG laser for the treatment of acne scars. A randomised plot-face clinical study. Journal of American Academy of Dermatology (2009)60, 801-807
- Hession MT, Graber EM; Atrophic Acne Scarring. Journal of Clinical and Aesthetic Dermatology (2015)8, 50-58
- Alexiades-Armenakas MR, Dover JS, Arndt KA; The spectrum of laser skin resurfacing: nonablative, fractional and ablative laser resurfacing. Journal of American Academy of Dermatology (2008)58, 719-717
- Sardana K, G VK, Arora P, Khurana N; Histological Validity and clinical evidence for use of fractional lasers for acne scars. Journal of Cutaneous and Aesthetic Surgery (2012)5, 75-90
- Rivera AE; Acne scarring: A review and current treatment modalities. Journal of American Academy of Dermatology (2008)59, 659-676
- Manuskiatti W, Triwongwaranat D, Varothai S, Eimpunth S, Wanitphakdeedecha R; Efficacy and safety of a carbon-dioxide ablative fractional resurfacing device for treatment of atrophic acne scars in asians. Journal of American Academy of Dermatology (2010)63, 274-283
- Hsiao PF, Lin YC, Huang CC, Wu YW; Efficacy and safety of a single treatment using a 10,600nm carbon dioxide fractional laser for mild-to-moderate atrophic acne scars in asian skin. Dermatologica Sinica (2013)31, 59-63
- Philipp CM, Scharschmidt D, Berlien HP; Laser treatment of scars and keloids – how we do it. Medical Laser Application (2008)23, 79-86


